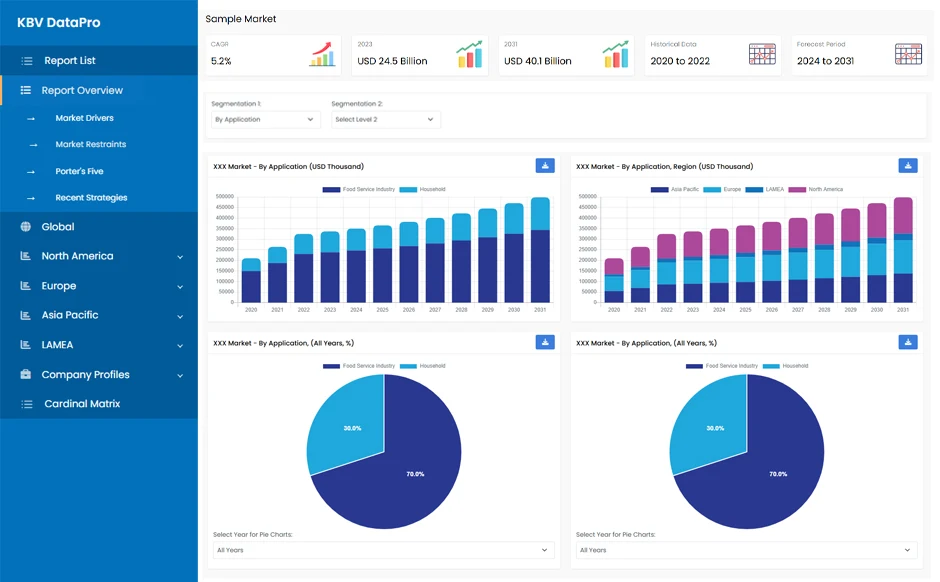
The Asia Pacific Healthcare Fraud Analytics Market would witness market growth of 23.7% CAGR during the forecast period (2022-2028).
Before alerts are sent to analysts, clinicians, or investigators, the system uses risk- and value-based scoring models to appropriately evaluate and prioritize them. Because of the time saved, valuable personnel can work on more cases with higher efficiency and concentrate on higher-value networks that generate a higher return on investment. More precise scoring also implies fewer false positives, which means less customer annoyance and more customer satisfaction.
With a powerful fraud analytics engine that examines all data in real-time or batch, organization can also detect more payment integrity violations than ever before. The solution, which runs on SAS Viya, combines advanced analytics with embedded artificial intelligence (AI) and machine learning algorithms, as well as other techniques such as outlier analysis, business rules, database searches, text mining, network link analysis, exception reporting, and so on, to uncover more suspicious activity with greater precision.
In Asia Pacific region, substantial number of population do have a health insurance, hence numerous people out of that population are found committing healthcare fraud with an objective of getting the lump sum insurance amount. Similarly, many skilled and qualified surgeons and other healthcare professionals are found making high level healthcare fraud with carefully designed schemes to conceal the fraud. The medical association of the region as well as the respective government of the region are bringing relevant policies and regulations to get rid of such healthcare frauds, but it is not enough as whole medical infrastructure of the region is demanding the incorporation of Healthcare Fraud Analytics System to systematically get rid of all kind of healthcare frauds by both patients and healthcare professionals.
The China market dominated the Asia Pacific Prescriptive Analytics Market by Country in 2021, and would continue to be a dominant market till 2028; thereby, achieving a market value of $116.5 million by 2028. The Japan market is Poised to grow at a CAGR of 23.6% during (2022 - 2028). Additionally, The India market would showcase a CAGR of 25.1% during (2022 - 2028).
Based on Delivery Model, the market is segmented into On-premise and Cloud. Based on Application, the market is segmented into Insurance Claim Review, Pharmacy billing Issue, Payment Integrity, and Others. Based on End User, the market is segmented into Public & Government Agencies, Private Insurance Payers, Third-party Service Providers, and Employers. Based on Solution Type, the market is segmented into Descriptive Analytics, Predictive Analytics, and Prescriptive Analytics. Based on countries, the market is segmented into China, Japan, India, South Korea, Singapore, Malaysia, and Rest of Asia Pacific.
Free Valuable Insights: The Worldwide Healthcare Fraud Analytics Market is Projected to reach USD 6.6 Billion by 2028, at a CAGR of 23%
The market research report covers the analysis of key stake holders of the market. Key companies profiled in the report include Wipro Limited, IBM Corporation, DXC Technology Company, SAS Institute, Inc., Conduent, Incorporated, HCL Technologies Ltd., UnitedHealth Group, Inc. (Optum, Inc.), OSP Labs, Cotiviti, Inc., and ExlService Holdings, Inc.
By Delivery Model
By Application
By End User
By Solution Type
By Country
Our team of dedicated experts can provide you with attractive expansion opportunities for your business.