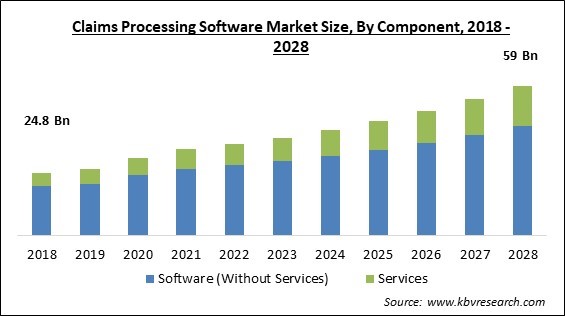
The Global Claims Processing Software Market size is expected to reach $59 billion by 2028, rising at a market growth of 8.5% CAGR during the forecast period.
Claims management software is software that allows businesses to create and execute automated end-to-end claims operations that are highly agile, intelligent, and ready to generate revenue. Companies become able to easily establish intelligent, dynamic business rules that completely capture company objectives as well as best practices, and then utilize those rules to drive automated processes that consistently apply the best thinking across enterprises using claims software. Customer-focused, cost-effective, and adaptable claims processing processes are required by insurers, healthcare professionals, and manufacturing enterprises.
Insurance claims processing software can be used by leading organizations within these industries in order to minimize operational inefficiencies and legacy difficulties, cut training and maintenance costs, and enhance the customer experience. Automated processes are as smart as the business regulations that drive them, and these platforms fulfill business requirements and capability that is significantly more sophisticated and flexible than competing alternatives. Claims processing software empowers businesses more than any other business management solution.
For instance, a medical claim is an invoice sent to a health insurance company by a doctor or medical facility after a patient has received treatment. It outlines the services a patient received as well as the charges imposed by the doctor or facility. These services are described using a large number of standardized medical codes known as Current Procedural Terminology (CPT) codes, which help to speed up the claims review and payment process.
Claims processing is a complex process with over 20 stages that each claim must pass through before being authorized. If a claim passes all of these checks with flying colors, the insurance company authorizes it and begins processing any insurance payouts. If it doesn't, it will either be rejected or returned for more information.
The COVID-19 pandemic has had a favorable impact on the claims processing software market since customers of health insurance as well as general insurance required claims settlement due to persistent health difficulties and business losses. The insurance companies found it difficult to cope with the unexpected increase in claim settlements, so they began to use claims processing software that could readily handle huge numbers of claims at once. Furthermore, it accelerated the process, saving personnel time and effort. As a result, during the COVID-19 pandemic, demand for insurance claims processing software surged.
Manual processes take a long time and are more prone to result in incorrect paperwork along with other administrative problems. Traditional claims management solutions are not only more prone to mistakes, but they can also become obsolete. One of the most significant advantages of claims processing software is that it completely eliminates the need for these manual processes. It cuts down on errors, saves time, and improves data accuracy. Any company's growth depends on its ability to organize and standardize its operations. The company's adjustment department should have established methods that everyone can follow.
Insurance claims management systems ensure that accurate data is processed, resulting in better service and increased customer satisfaction. It enables insurance companies to compete successfully in the market by eliminating manual mistake. By automating the entire process, it is possible to reduce and eliminate human error. This helps employees save time and increase their productivity, allowing them to better serve their clients. The software intelligently extracts specific data items to make integration easier, then evaluates them against the policy. It sends out multi-level notifications automatically and efficiently raises alerts for unrecognized loss reports.
Claims processing software is a very efficient and effective solution for the management of claims processing procedures. It significantly saves time and the cost of an enterprise. However, the initial cost of acquiring necessary hardware and software is a key barrier to the migration of enterprises from traditional claims processing to contemporary and automated claims processing software. Training for the entire workforce to learn how to enter and utilize the software is another add-on to the start-up cost. Once the system is in place, all client records must be transferred to electronic format, which takes a lot of time and money to do.
Based on Component, the market is segmented into Software (Without Services) and Services. In 2020, the software (without services) segment acquired the largest revenue share of the claims processing software market. The growth of the segment is increasing due to claim processing software's ability to provide a full perspective of claims, making it easier to identify discrepancies and detect potential fraud early on. Furthermore, claims processing software is far more capable of detecting errors than the human eye.
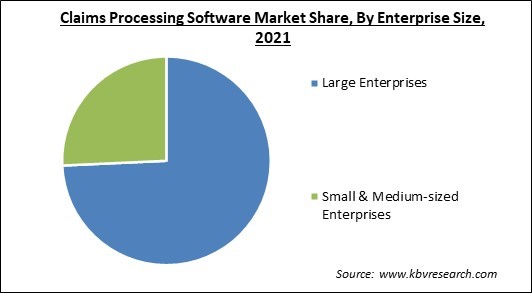
Based on Enterprise Size, the market is segmented into Large Enterprises and Small & Medium-sized Enterprises. In 2021, the small and medium-sized enterprises segment witnessed a substantial revenue share of the claims processing market. The expediting growth of this segment is attributed to the cost-efficiency of claims processing software. This software significantly saves time and allows the organization to leverage that time in any other operation.
Based on End User, the market is segmented into Insurance Companies, Insurance Intermediaries, Agents & Brokers, and Others. In 2020, the insurance companies segment registered the largest revenue share of the claims processing software market. This is due to the fact that the insurance claims management system enables insurance businesses to function more efficiently by providing faster access to claims data. The program also enables increased process visibility by tracking the performance of claim processes.
| Report Attribute | Details |
|---|---|
| Market size value in 2021 | USD 34 Billion |
| Market size forecast in 2028 | USD 59 Billion |
| Base Year | 2021 |
| Historical Period | 2018 to 2020 |
| Forecast Period | 2022 to 2028 |
| Revenue Growth Rate | CAGR of 8.5% from 2022 to 2028 |
| Number of Pages | 209 |
| Number of Tables | 343 |
| Report coverage | Market Trends, Revenue Estimation and Forecast, Segmentation Analysis, Regional and Country Breakdown, Companies Strategic Developments, Company Profiling |
| Segments covered | Component, Enterprise Size, End User, Region |
| Country scope | US, Canada, Mexico, Germany, UK, France, Russia, Spain, Italy, China, Japan, India, South Korea, Singapore, Malaysia, Brazil, Argentina, UAE, Saudi Arabia, South Africa, Nigeria |
| Growth Drivers |
|
| Restraints |
|
Based on Regions, the market is segmented into North America, Europe, Asia Pacific, and Latin America, Middle East & Africa. In 2020, North America accounted for the largest revenue share of the claims processing market. This is due to the fact that North America has seen a higher rate of adoption of cloud-based solutions as a result of growing digitalization in the insurance and e-commerce sectors, which boosts the regional market's growth potential significantly.
Free Valuable Insights: Global Claims Processing Software Market size to reach USD 59 Billion by 2028
The market research report covers the analysis of key stake holders of the market. Key companies profiled in the report include Duck Creek Technologies, Inc., FINEOS Corporation Holdings plc, Hyland Software, Inc., Hawksoft, Inc., HIPAAsuite, Newgen Software Technologies Limited, Pegasystems, Inc., Quick Silver Systems, Inc., Ventiv Technology, and A1 Enterprise, Inc.
By Component
By Enterprise Size
By End User
By Geography
The global Claims Processing Software market size is expected to reach $59 billion by 2028.
Increased Productivity and Standardization along with the reduced cost are driving the market in coming years, however, higher initial and maintenance cost of claims processing software limited the growth of the market.
Duck Creek Technologies, Inc., FINEOS Corporation Holdings plc, Hyland Software, Inc., Hawksoft, Inc., HIPAAsuite, Newgen Software Technologies Limited, Pegasystems, Inc., Quick Silver Systems, Inc., Ventiv Technology, and A1 Enterprise, Inc.
The COVID-19 pandemic has had a favorable impact on the claims processing software market since customers of health insurance as well as general insurance required claims settlement due to persistent health difficulties and business losses.
The Large Enterprises segment is leading the Global Claims Processing Software Market by Enterprise Size in 2021, thereby, achieving a market value of $42.09 billion by 2028.
The North America market dominated the Global Claims Processing Software Market by Region in 2021, and would continue to be a dominant market till 2028; thereby, achieving a market value of $26.5 billion by 2028.
Our team of dedicated experts can provide you with attractive expansion opportunities for your business.